Thursday, August 31, 2006
If your In the Area?
I will be involved with Alyssa's and Trevor's birthdays on Friday and Saturday night. We will celebrate both on Sunday PM with Kathy. If you would like to visit with Kathy any of these afternoons or evenings I would welcome it! Thanks for the prayers and love!
It's Been a Hard Days Night
The good new is Kathy has moved on to rehabilitation! That means the immediate threat of her brain abscess recovery and pneumonia has been reduced to a management status. As I am writing this blog she is hard asleep.
The Sharp medical staff has spent the day validating everything from Scripps documents. Since the responsibility is on Sharp to maintain her at a high level, they need to do their own analysis and due diligence. I will find out more tomorrow when I meet with her case manager.
Information on her stay at Sharp Rehabilitation Center:
Sharp Rehabilitation Center
2999 Health Center Drive
San Diego, California 92121
Room 148
Room Telephone Number 858-939-4729 (She probably cannot answer the phone until Tuesday due to her strength)
Talking to the staff they prefer visitors to come from NOON until 10:00 PM daily. She is involved in daily therapy form morning until 4:00 PM daily. They will give her light therapy on Saturdays and Sundays off. They encourage visitors to come in the late evenings/nights or on the weekends.
The Sharp medical staff has spent the day validating everything from Scripps documents. Since the responsibility is on Sharp to maintain her at a high level, they need to do their own analysis and due diligence. I will find out more tomorrow when I meet with her case manager.
Information on her stay at Sharp Rehabilitation Center:
Sharp Rehabilitation Center
2999 Health Center Drive
San Diego, California 92121
Room 148
Room Telephone Number 858-939-4729 (She probably cannot answer the phone until Tuesday due to her strength)
Talking to the staff they prefer visitors to come from NOON until 10:00 PM daily. She is involved in daily therapy form morning until 4:00 PM daily. They will give her light therapy on Saturdays and Sundays off. They encourage visitors to come in the late evenings/nights or on the weekends.
Wednesday, August 30, 2006
Frequently Asked Questions About Sharp Rehabilitation

Frequently Asked Questions About Sharp Rehab
Sharp Rehabilitation Services — From Possibility to Ability
For nearly 45 years Sharp Rehabilitation Center has provided comprehensive inpatient and outpatient rehabilitation services to Southern Californians.
Our continuum of rehabilitation care includes programs and services designed to address all types of injuries and illness. From the basic orthopedic injuries to complex conditions, such as stroke, brain injury and spinal cord injury, Sharp provides specialized programs and services to meet each individual’s needs. In addition, Sharp is the leader in providing support services to families and care-givers.
The following are some of the more frequently asked questions.
What type of patients do you serve?
Age range is between 14 and 90 +. Regardless of injury or illness, patients are seen if they have physical and cognitive functional limitations that can benefit from our services.
What types of inpatient services are offered?
All programs and services are individualized with your treatment team. The team is lead by a Physiatrist (physician that specializes in Rehabilitation) and includes nurses, physical, occupational, speech and occupational therapists. Other team members include social workers, psychologists, case managers and discharge planners. The patient and family are at the center of the team. Your team will meet at regular intervals to review your progress.
What types of specialized programs are offered?
Sharp rehab offers specialized programs for stroke, brain injury, spinal cord and other neuro musculoskeletal injuries.
How does inpatient rehabilitation differ from an acute hospital?
Patients and families should understand that an inpatient rehabilitation is different than an Intensive Care hospital setting. During the first 24 hours at an inpatient rehabilitation center, patients will receive an extensive assessment from various health care professionals to determine their physical, therapeutic and psychological needs. Following this assessment, and in collaboration with the patient and family, an aggressive “plan of care” is developed.
Once the plan of care is outlined, patients are expected to work hard to participate in scheduled therapies and educational programs. Families and care givers are also encouraged to participate. This insures that the patient and family receive the most from their time spent in the rehabilitation program.
How long do patients stay for inpatient rehabilitation services?
Length of stay is based on each individual’s treatment goals and determined by the rehabilitation team. The rehabilitation treatment team continually monitors the patient’s progress and works with the patient and family/care-giver in preparing for discharge. Currently, our average length of stay is approximately 19 days. Depending on type of injury, length of stay can range from 10 - 40 days.
What happens after discharge?
Sharp offers an extensive list of outpatient therapy programs and services to help patients increase functional abilities. These services may be offered here at Sharp Memorial rehabilitation Center or at our other rehabilitation centers located through out San Diego County. In addition to therapy services, Sharp offers a variety of support activities and groups to help with re-integration into community living.
Is the cost of Inpatient Rehabilitation covered by my insurance?
In most cases the answer is “yes”. However, health insurance is more complex than ever before. Sharp will provide a knowledgeable and experienced staff to address insurance questions and concerns.
How do you measure your success?
Several measures are tracked to determine success. Upon admission to the Rehabilitation Center, every inpatient is rated on their abilities to perform activities such as dressing, mobility, communication. Through-out the inpatient rehabilitation stay, progress measured and tracked and at discharge, each patient is rated and increased functional ability is documented.
83% of our patients return to home at discharge. After discharge, each patient is contacted to determine their status and progress and to measure their level of satisfaction with the services they received. During 2005, our patient satisfaction scores were as follows:
94.1% Overall patient satisfaction
94.3% Likely to recommend Sharp Rehab to others
95.4% Sharp Rehab Program helped you reach your goals
The Razor's Edge
The eagle has landed. After all the gymnastics, we have finally gotten Kathy into Sharp Rehabilitation. Sharp Rehabilitation is one of the best facilities in the county and has quite a reputation for excellence. Tomorrow at 10:00 AM, Mercy Hospital will transport Kathy to Sharp and get her checked in. After touring the facility yesterday, I feel Kathy should excel in this type of team work environment.
Today Kathy was poked, pushed and tested to her abilities. She again was issued high marks from her infection disease doctor and pulmonary doctor. They are amazed at her success and truly enjoy checking up on her. She successfully completed her limited therapy today and she looks forward to the acute care she will receive in her new facility. GOOOOOOOOOOOO KAAAAAAAAATTTHHHYYYY!
Today Kathy was poked, pushed and tested to her abilities. She again was issued high marks from her infection disease doctor and pulmonary doctor. They are amazed at her success and truly enjoy checking up on her. She successfully completed her limited therapy today and she looks forward to the acute care she will receive in her new facility. GOOOOOOOOOOOO KAAAAAAAAATTTHHHYYYY!
Tuesday, August 29, 2006
Rancho Levels Of Cognitive Functioning
Not at bedside, some of you might wonder how Kathy's mental recovery is progressing. A good tool is the "Rancho Levels of Cognitive Functioning" scale reported earlier in my blog. After review (1 to 10 highest) , I would guess Kathy tonight is a strong level 6.
After reading the scale closer, a lot of people I have run into over the years do not even meet level 9 or 10 ! My gut feeling is Kathy is much more on top of things than she lets on and is sometimes masking her progress with emotional duress and fatigue. The biggest road blocks lies ahead is not her mental recovery but probably getting her strength back and balancing her right and left side. We all know one thing about Kathy, this probably is the easiest road block ahead!
My Conclusion: READ BELOW
Level 6 Confused-appropriate Assistance
Inconsistently oriented to person, and place. Able to attend to highly familiar tasks in non-distracting environment for 30 minutes with moderate redirection. Remote memory has more depth and detail than recent memory. Vague recognition of some staff. Able to use assistive memory aide with maximal assistance. Emerging awareness of appropriate response to self, family and basic needs. Emerging goal directed behavior related to meeting basic personal needs. Moderate assistance to problem solve barriers to task completion. Supervised for old learning (e.g. self care). Shows carry over for relearned familiar tasks (e.g. self care). Maximal assistance for new learning with little or no carry over. Unaware of impairments, disabilities and safety risks. Consistently follows simple directions. Verbal expressions are appropriate in highly familiar and structured situations
After reading the scale closer, a lot of people I have run into over the years do not even meet level 9 or 10 ! My gut feeling is Kathy is much more on top of things than she lets on and is sometimes masking her progress with emotional duress and fatigue. The biggest road blocks lies ahead is not her mental recovery but probably getting her strength back and balancing her right and left side. We all know one thing about Kathy, this probably is the easiest road block ahead!
My Conclusion: READ BELOW
Level 6 Confused-appropriate Assistance
Inconsistently oriented to person, and place. Able to attend to highly familiar tasks in non-distracting environment for 30 minutes with moderate redirection. Remote memory has more depth and detail than recent memory. Vague recognition of some staff. Able to use assistive memory aide with maximal assistance. Emerging awareness of appropriate response to self, family and basic needs. Emerging goal directed behavior related to meeting basic personal needs. Moderate assistance to problem solve barriers to task completion. Supervised for old learning (e.g. self care). Shows carry over for relearned familiar tasks (e.g. self care). Maximal assistance for new learning with little or no carry over. Unaware of impairments, disabilities and safety risks. Consistently follows simple directions. Verbal expressions are appropriate in highly familiar and structured situations
Pick of the Litter
Today I visited two potential physical rehabilitation sites for Kathy’s recovery. First I visited Sharp Rehabilitation and afterwards San Diego Rehabilitation Institute. Sharp has a well respected program and the hospital is rated high on most surveys. The rehabilitation equipment and rooms seemed extensive and first class. They have a specialized brain injury department with respective therapy equipment. San Diego Rehabilitation’s program seemed less extensive and modern. I liked the way the hospital was laid out and the rooms are better than Sharps. The people seemed friendlier but SDR does not have the reputation or the equipment that Sharp’s posses. The new rehabilitation nurse thought highly of Scripps Encinitas rehabilitation facility (she worked there for 10 years) and I will add that to my list. Too Confusing?
Kathy’s voice came out clearer with her speech therapist this morning. Later in the day she did about a half hour of physical therapy and was very weak when attempting to sit up or stand for a few minutes. (She is going to need lots of therapy to get her standing after three weeks in bed) Her respiratory doctor swung by and said her pneumonia is under control and he expects it to be gone in a few days. She slept the afternoon
This evening we made calls to family members and friends and Kathy seems very understanding of each conversations. She responds as if she was having a normal conversation but with a very weak voice. This is quite unusual because rarely will she talk to anyone in her presence like she does on the phone. Maybe because she can use visual feedback like eye movement and hand signs she chooses not to engage? The phone requires her to say something to the other party on the line?
Kathy’s case manager thinks she will be OK to transfer to a rehabilitation facility in the next two to three days…..
Kathy’s voice came out clearer with her speech therapist this morning. Later in the day she did about a half hour of physical therapy and was very weak when attempting to sit up or stand for a few minutes. (She is going to need lots of therapy to get her standing after three weeks in bed) Her respiratory doctor swung by and said her pneumonia is under control and he expects it to be gone in a few days. She slept the afternoon
This evening we made calls to family members and friends and Kathy seems very understanding of each conversations. She responds as if she was having a normal conversation but with a very weak voice. This is quite unusual because rarely will she talk to anyone in her presence like she does on the phone. Maybe because she can use visual feedback like eye movement and hand signs she chooses not to engage? The phone requires her to say something to the other party on the line?
Kathy’s case manager thinks she will be OK to transfer to a rehabilitation facility in the next two to three days…..
Monday, August 28, 2006
Manic Monday
Kathy had a busy Monday with everybody at Scripps back at their posts. She had visits with her pulmonary doctor, her infectious disease doctor, her primary doctor, her medication doctor, her team doctors from ICU, her RN, her RN assistant, her breathing treatment technician, her speech trainer her physical trainer and her San Diego Rehab facilitator all in 4 hours! Great News! They were all pleased with her appearance and progress over the weekend!
Physically, her pneumonia remains a threat but she is breathing steady and seems to be on an upswing. (Please don't move her and screw this up) Her bacteria cultures remain negative for blood, urine and brain fluids. About the only thing wrong is she says she is a tad warm but her temps remain around 97-98 degrees.
Mentally, Kathy is a becoming a classic case of brain trauma recovery. She knows things are not right and is worried. We try to give her hourly accolades and "thata girls" but she knows it's going to be a battle. Lately, I finding it more time intensive and difficult to keep Kathy positive and focused. The good news, Kathy has spirit and is trying hard every day.
Tomorrow I am going to check out Sharp Rehabilitation (I've heard good things) and make sure I'm making the best possible choice. Kathy had great fun today, listening to her iPod, getting books and magazine read to her and a throng of evening visitors to bolster her. Thanks to all of you!
Physically, her pneumonia remains a threat but she is breathing steady and seems to be on an upswing. (Please don't move her and screw this up) Her bacteria cultures remain negative for blood, urine and brain fluids. About the only thing wrong is she says she is a tad warm but her temps remain around 97-98 degrees.
Mentally, Kathy is a becoming a classic case of brain trauma recovery. She knows things are not right and is worried. We try to give her hourly accolades and "thata girls" but she knows it's going to be a battle. Lately, I finding it more time intensive and difficult to keep Kathy positive and focused. The good news, Kathy has spirit and is trying hard every day.
Tomorrow I am going to check out Sharp Rehabilitation (I've heard good things) and make sure I'm making the best possible choice. Kathy had great fun today, listening to her iPod, getting books and magazine read to her and a throng of evening visitors to bolster her. Thanks to all of you!
Sunday, August 27, 2006
Visiting on Monday and Tuesday
If you want to visit Kathy, I could use the help when I am not there. I will be with Kathy in the morning Monday but no coverage in the afternoon or evening. On Tuesday I will be with Kathy in the afternoon and evening. Of course any visit will be appreciated!
She will have rehabilitation during the day and in most cases you are welcome to stay!
Again, thanks for the prayers and support for Kathy-WE LOVE HER
She will have rehabilitation during the day and in most cases you are welcome to stay!
Again, thanks for the prayers and support for Kathy-WE LOVE HER
Remote!
Sunday Kathy seemed to be relaxed and stable. They moved her from the 10th floor to the 6th floor and twice on the 6th floor. She currently is in room 606. (Thanks-not 666) All her vitals are good with plenty of oxygenation and a steady heart rate. She does seem to have a little shake in her hands and right leg that is bothersome. Overall her physical condition, even with pneumonia, is getting incrementally better. When you walk in the door, immediately Kathy looks like she’s feeling better and more rested.
The mental picture is a little more complicated. I’m sure it will take time and lots of frustration. Kathy tends to loose interest in minute to minute events but sure likes her TV! I don’t know why, but I think the constant change of pace on the TV screen keeps her attention. She does recognize people and understand what you’re talking about but does not seem super interested. She is right now controlling the TV and having a glycerin stick.
Tomorrow, Kathy will get back into all of her therapy; physical, swallowing, speech and breathing. Sometime tomorrow, they will give us more information on when she will be transferred to San Diego Rehabilitation. IF ANY OF YOU know stories of good or bad on San Diego Rehab, Continental Rehab, Sharp Rehab or Palomar Rehab, I would appreciate it. I hope to make a run to personally visit the facilities tomorrow.
The mental picture is a little more complicated. I’m sure it will take time and lots of frustration. Kathy tends to loose interest in minute to minute events but sure likes her TV! I don’t know why, but I think the constant change of pace on the TV screen keeps her attention. She does recognize people and understand what you’re talking about but does not seem super interested. She is right now controlling the TV and having a glycerin stick.
Tomorrow, Kathy will get back into all of her therapy; physical, swallowing, speech and breathing. Sometime tomorrow, they will give us more information on when she will be transferred to San Diego Rehabilitation. IF ANY OF YOU know stories of good or bad on San Diego Rehab, Continental Rehab, Sharp Rehab or Palomar Rehab, I would appreciate it. I hope to make a run to personally visit the facilities tomorrow.
Information on Kathy's Rehabilitation Facility

Kathy's next stop!
Web Address:http://www.alvaradohospital.com/CWSContent/alvaradohospital/ourServices/medicalServices/SanDiegoRehab
San Diego Rehabilitation Institute
Inpatient: (619) 229-7380
6655 Alvarado Road, San Diego CA 92120
Suffering a disability or having a loved one suffer a disability can be a devastating experience. There are so many things to consider such as finding the care and support to help restore the quality of life that is often taken away. That’s why at the San Diego Rehabilitation Institute (SDRI), we specialize in striving to restore patients to a high quality of life after experiencing disability.
As one of the greater San Diego area’s leading centers of comprehensive rehabilitation services, SDRI’s team of dedicated professionals understands what the challenges of disability are. We have the skills and specialized programs to prepare our patients for their return to home, family and employment. Our success has been built on honest, cooperative relationships with our patients, their families, physicians, employers and insurance companies. We believe that a team effort is critical to our patients’ success and we strive to work closely with all parties for quality treatment for our patients.
Transitional Care
SDRI’s 30-bed Transitional Care Unit (TCU) offers both medical and rehabilitative services. The TCU provides short-term skilled nursing care for people who do not require the entire resources of an acute hospital but still require 24-hour nursing care. The unit also provides a link in the progressive recovery of patients who are recuperating from a condition that requires rehabilitative specialists. Our goal is to deliver quality medical and rehabilitative care in a cost-efficient manner in a comfortable and caring environment.
Some of the medical conditions we treat in the TCU include:
Diabetic complications
Surgical aftercare
Persistent infections
Infusion therapy
Wound and burn care
Organ transplant aftercare
General skilled nursing
Some of the rehabilitation conditions we treat in the TCU include:
Spine/back conditions
Joint replacements
Orthopedics and multi-trauma injuries
Cardio-pulmonary conditions
Neuromuscular diseases
Neurological conditions
Get Out of that Funk
Kathy is remaining in ICU today because of the shortage of staff on the 11th floor. Kathy’s pneumonia is improving slightly and the doctors feel she is doing good enough to not only get out of ICU but then go to rehabilitation. They estimate a few days to stabilize on the 11th floor and by Tuesday or Wednesday she will transported to rehabilitation. She has been approved to go to San Diego Rehabilitation where she will spend upwards of 3-4 hours daily of physical and mental rehabilitation.
Kathy’s metal side is pretty alert which makes her susceptible to the ups and downs of daily hospital life. She expresses all the feelings, happy, bored, tired or in pain. Lately she has been slightly depressed so today I hope top cheer her up by bringing in her iPod, pictures and magazines. Her emotional side is down so I have to remind myself to not put too much on the table.
The seeming good news is the most serious physical dangers are behind us. We need to keep a watchful eye on the pneumonia and hope for the bacteria issues to stop. All her cultures remain negative at the moment. Her Doctor came by yesterday afternoon and wanted to get her dentist's telephone number so he could discuss with him the possible causes of the abscess. He reminded me that Kathy will have to take antibiotics for the next 6 months at least. Heading off with the goodies….
Kathy’s metal side is pretty alert which makes her susceptible to the ups and downs of daily hospital life. She expresses all the feelings, happy, bored, tired or in pain. Lately she has been slightly depressed so today I hope top cheer her up by bringing in her iPod, pictures and magazines. Her emotional side is down so I have to remind myself to not put too much on the table.
The seeming good news is the most serious physical dangers are behind us. We need to keep a watchful eye on the pneumonia and hope for the bacteria issues to stop. All her cultures remain negative at the moment. Her Doctor came by yesterday afternoon and wanted to get her dentist's telephone number so he could discuss with him the possible causes of the abscess. He reminded me that Kathy will have to take antibiotics for the next 6 months at least. Heading off with the goodies….
Saturday, August 26, 2006
Where's Waldo?
The Scripps Mercy shell game is on. On Wednesday they moved Kathy from the second floor ICU to the eleventh floor regular. They then moved her twice to get her to a private room. On Thursday they moved her back to ICU on the second floor. On Friday they moved her from the ICU on the second floor to the ICU on the tenth floor. She is currently on the tenth floor. Rumored today she is moving to the eleventh floor. That will be 5 moves in 4 days!
If you plan to visit, please be patient and hope they don’t lose her!
If you plan to visit, please be patient and hope they don’t lose her!
A Walk in the Park
Yesterday was a good day for all of us. Kathy responded in ICU to her intensive care and medication. Dr. Ballon-Landa, her infections specialist, continued to give her new combinations of antibiotics to improve her condition. Kathy pneumonia, luckily, is limited to one lung and with breathing treatments every three to four hours, she was breathing easier. Mentally, Kathy is pretty much back to her peak progress showed on Wednesday. She's alert to conversation and even attempts to comment or talk when she wants to make a statement.
What next? Well, today if Kathy keeps up her strong recovery, they will want her to move back to 11th floors (Hell level) for the next few days. If the nurses on floor 11 don’t make mistakes and put Kathy back into ICU, she should move on to a rehabilitation hospital in a few days. At the rehabilitation hospital, they supply acute care, but more importantly provide Kathy with 3-4 hours of therapy to improve speech, memory and her range of movement. Scripps advised us she would probably need around (2) weeks in rehabilitation before coming home. At home she would need some assistance until she feels comfortable.
Macy suggested two facilities near Mercy hospital, San Diego Rehabilitation (Macy’s old haunt) or Continental, located across the street. I am going to check out both this weekend to find the best for Kathy.
This morning, the nurse reported Kathy had a good night, got her bath and hair shampooed and is looking beautiful. (Kathy told me last night she wanted to cut her hair off-I think people’s comments are making her feel self conscious about her hair) She had a strong headache (?) and they gave her Imitrix, her migraine medicine. She was sleeping well this morning……….
What next? Well, today if Kathy keeps up her strong recovery, they will want her to move back to 11th floors (Hell level) for the next few days. If the nurses on floor 11 don’t make mistakes and put Kathy back into ICU, she should move on to a rehabilitation hospital in a few days. At the rehabilitation hospital, they supply acute care, but more importantly provide Kathy with 3-4 hours of therapy to improve speech, memory and her range of movement. Scripps advised us she would probably need around (2) weeks in rehabilitation before coming home. At home she would need some assistance until she feels comfortable.
Macy suggested two facilities near Mercy hospital, San Diego Rehabilitation (Macy’s old haunt) or Continental, located across the street. I am going to check out both this weekend to find the best for Kathy.
This morning, the nurse reported Kathy had a good night, got her bath and hair shampooed and is looking beautiful. (Kathy told me last night she wanted to cut her hair off-I think people’s comments are making her feel self conscious about her hair) She had a strong headache (?) and they gave her Imitrix, her migraine medicine. She was sleeping well this morning……….
Friday, August 25, 2006
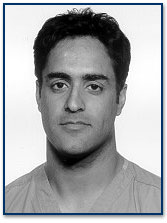
Kathy's Internal Bacteria Specialist

Dr. Ballon-Landa was board certified in Internal Medicine in 1980. He was also board certified in Infectious Disease in 1984. Dr. Ballon-Landa received his medical degree from Northwestern University in Chicago in 1977. He is a past president of the Infectious Diseases Association of California, and is a councillor in the board of the Infectious Diseases Society of America. He received the prestigious "Clinician Award"
Above is the Doctor that is working on different combinations of penicillin and antibiotics to treat Kathy. He is considered one of the best in the business. Keep up the good work Doc!
Pneumonia
I called Kathy’s nurse Rachael this morning and she was doing better breathing and seemed more comfortable. Her CT scan of the lung last night was not good and confirmed a severe case of pneumonia. Her pneumonia is affecting her one lung in the lower lobe and the other lung in the upper lobe. About the only good thing to report is, she has not gone on a ventilator and her vitals are steady.
Her blood bacteria cultures are not taking so they think she might have cleared up but it will take a few more days to review the cultures. Her culture on her brain fluid does show bacteria and they are taking a more intensive approach.
Kathy’s nurse is concerned she has so many things going on and is worried about a quick outcome. She cannot predict how and when she will improve. She also noted that Kathy seemed down in her sprits and I hope we can get her BACK UP today. Whoever sent flowers, thank you! I have to pick them up from the 11th floor and take them home because in ICU you cannot have flowers.
Her blood bacteria cultures are not taking so they think she might have cleared up but it will take a few more days to review the cultures. Her culture on her brain fluid does show bacteria and they are taking a more intensive approach.
Kathy’s nurse is concerned she has so many things going on and is worried about a quick outcome. She cannot predict how and when she will improve. She also noted that Kathy seemed down in her sprits and I hope we can get her BACK UP today. Whoever sent flowers, thank you! I have to pick them up from the 11th floor and take them home because in ICU you cannot have flowers.
Thursday, August 24, 2006
Conspiracy Theory
Kathy seems to have fallen victim to the hospital curse. Today she was being pushed hard by speech therapy to eat solid food for lunch and she eventually got some of these gastric juices into her lungs. Shoot, she wasn't even allowed to drink water but they wanted her to eat solid foods! Obviously, this got down into her lungs accelerating damage to her lungs.
The doctors spent the afternoon giving Kathy breathing treatments and injections of medicines to improve her intake of oxygen. She showed so little improvement combined with severe congestion, she was put back into ICU for safety. She is set up to have a lung CT tonight.
This is two steps back and one step forward! I am totally upset and fustrated because Kathy was so close on Monday to breaking out and heading for full recovery.
Kathy is in non surgical ICU (acronymsm NSICU -acrosss from surgical ICU). After visiting her room tonight she is in good hands. (I am actually relieved) The 11th floor medical coverage had a lot to be desired. Everyone here is trying their best but the demons of the hospital are taking there toll.
The doctors spent the afternoon giving Kathy breathing treatments and injections of medicines to improve her intake of oxygen. She showed so little improvement combined with severe congestion, she was put back into ICU for safety. She is set up to have a lung CT tonight.
This is two steps back and one step forward! I am totally upset and fustrated because Kathy was so close on Monday to breaking out and heading for full recovery.
Kathy is in non surgical ICU (acronymsm NSICU -acrosss from surgical ICU). After visiting her room tonight she is in good hands. (I am actually relieved) The 11th floor medical coverage had a lot to be desired. Everyone here is trying their best but the demons of the hospital are taking there toll.
Answers to Monday's Question

What do Randy D. Haskell and Kathleen D. Newhouse have in common?
Both had fathers in the avocado business
Both lived as teenagers in Valley Center
Both went to Orange Glenn High School
Both had employment connections to West Pak Avocado
Both have Bob and Debbie Shuford as friends
Both have the same Neurosurgeon: Dr. Kureshi
Both had surgeries in Mercy Hospital
That is 7 things in common at least! I don’t know how to call a clear winner here. Maybe a good consolidation prize is warranted! Thanks
Morning Update and Room Change
I talked to Kathy’s nurse this morning and she said everything went well last night. Really nothing to report except they will be drawing samples this morning to see how the infection is progressing.
Kathy has been moved out of ICU into a private room, 1101. The room is located on the llth floor of the main hospital building. Official visiting hours are 12:00 PM to 10:00 PM everyday. When Kathy has no work scheduled the nurse said visitors could come by as early as 9:00 AM. Her nurse recommended visiting after 10:00 AM.
Visiting will be more convenient because she has a private room with less stringent rules and regulations.
Kathy has been moved out of ICU into a private room, 1101. The room is located on the llth floor of the main hospital building. Official visiting hours are 12:00 PM to 10:00 PM everyday. When Kathy has no work scheduled the nurse said visitors could come by as early as 9:00 AM. Her nurse recommended visiting after 10:00 AM.
Visiting will be more convenient because she has a private room with less stringent rules and regulations.
Wednesday, August 23, 2006
Two Steps Forward and ONE STEP BACK!
As the saying goes today was that one step back. Kathy started the day out with optimism. Her brain tube was removed and stitched over, the team raved about her progress and she was being moved out of ICU. But the whammy hit! Kathy took a late morning nap waking up to a fever, fast breathing, fast heart rate and disoriented. Her disoriention was so bad she would barely respond to the nurses instructions. What had gone so wrong in a few hours?
Her fever was suspected to have caused the disoriention but where was the fever coming from? The doctors took a CT scan and found nothing, they took blood and urine samples looking for bacteria. The blood came back positive. Did Kathy have a blood infection? How could this be possible with so many antibiotics going through her? Did she get infected when they took out her tube or did something in ICU give her the infection? Did she have Sepia (blood infection) or was it something else?
Not getting a detailed response from her doctors tonight, we cannot be sure. All I know is, Kathy regressed in a big way today until she rallied tonight to come back within 50% of her morning progress. I just hope her progress continues overnight and we get a good explanation tomorrow. Kathy's fever is down and her medications have been changed. I constantly read and hear the best way to stop any infection is getting quick treatment and Kathy did so. Keep your fingers crossed.
Her fever was suspected to have caused the disoriention but where was the fever coming from? The doctors took a CT scan and found nothing, they took blood and urine samples looking for bacteria. The blood came back positive. Did Kathy have a blood infection? How could this be possible with so many antibiotics going through her? Did she get infected when they took out her tube or did something in ICU give her the infection? Did she have Sepia (blood infection) or was it something else?
Not getting a detailed response from her doctors tonight, we cannot be sure. All I know is, Kathy regressed in a big way today until she rallied tonight to come back within 50% of her morning progress. I just hope her progress continues overnight and we get a good explanation tomorrow. Kathy's fever is down and her medications have been changed. I constantly read and hear the best way to stop any infection is getting quick treatment and Kathy did so. Keep your fingers crossed.
Tuesday, August 22, 2006
Prognosis Up
All indicators were up on Kathy’s prognosis today. She had her CT scan early morning and everything was good. Dr. Kureshi will pull her pressure tube out tonight when he does his evening rounds. Most of the day I spent back at work and I am not able to give you much news. We did show up late in the afternoon and she was with her speech therapist. Everything went well with Kathy, she was able to do complex assignments and even write out words when words were tough to pronounce. She finished her session on a high note writing my name when asked who her sugar daddy was! We came back later this evening and Kathy was asleep, her back giving her some problems. Hope to work out that situation Wednesday morning with her pain management doctors. Keep up the prayers please-there definitely working!
Monday, August 21, 2006
Best Times to Visit Kathy
Kathy is still weak and people have asked me how not to overload her. The best thing is visitors not to trickle in during the whole day but visit her when she is the most rested. I will return to a limited work schedule on Tuesday, Thursday and Saturday of this week. This will allow people to visit Kathy in the mornings when she is the most rested. Also, around 4:00 PM she is alert and again at 8:00 PM after shift change. Please feel free to call me anytime about anything!Thank again for your wonderful support and prayers!!
Getting Better Every Day
Last night Kathy got a CT scan and everything looked good. She continues to have a lot of junk in her lungs that the breathing specialist works on four times a day to get up and out. She did not pass her physical therapist tests this afternoon so she must stay on the feeding tube until tomorrow. Overall her condition remains good physically, low brain pressure, decreased white cell count, moderate use of medication, good breathing, steady heartbeat and normal temperature. The only thing she is behind on is her right side catching up with her left side’s dexterity.
Her mental condition continues to improve with less sleeping, more concentration, good reflex to commands, ability to be cognizant of her visitors and what they say, speaking small sentences and good recall of her memories. She currently is under the care of a full time nurse, neurologist, internal medicine doctor, a physical therapist, breathing therapist, speech therapist, transition administrator and numerous others. She is in good hands.
Hopefully tomorrow the planned CT scan will allow Dr. Kureshi to remove her brain tube and passing tomorrow's speech therapist test will allow removal of her feeding tube-no more tubes! This landmark will allow her to transition out of CUI into general care. We had an interesting visit this afternoon from one of her original admitting doctors. She had a special attachment to Kathy because she had earlier in her life experienced a brain abscess exactly like hers. She told us that Kathy had gotten Staphylococci bacteria most likely from her mouth area and the size of the abscess was around 2 cm in size, growing left to right. She was glad to see Kathy have a miracle because she thought her swelling was so severe, she might not make it. She’s so exited and wants to later share her experiences with Kathy.
Again “A laymen’s description of a brain abscesses”:
“Brain abscesses commonly occur when bacteria or fungi infect part of the brain. Inflammation develops in response. Infected brain cells, white blood cells, and live and dead microorganisms collect in a limited area of the brain. This area becomes enclosed by a membrane that forms around it and creates a mass.”
Her mental condition continues to improve with less sleeping, more concentration, good reflex to commands, ability to be cognizant of her visitors and what they say, speaking small sentences and good recall of her memories. She currently is under the care of a full time nurse, neurologist, internal medicine doctor, a physical therapist, breathing therapist, speech therapist, transition administrator and numerous others. She is in good hands.
Hopefully tomorrow the planned CT scan will allow Dr. Kureshi to remove her brain tube and passing tomorrow's speech therapist test will allow removal of her feeding tube-no more tubes! This landmark will allow her to transition out of CUI into general care. We had an interesting visit this afternoon from one of her original admitting doctors. She had a special attachment to Kathy because she had earlier in her life experienced a brain abscess exactly like hers. She told us that Kathy had gotten Staphylococci bacteria most likely from her mouth area and the size of the abscess was around 2 cm in size, growing left to right. She was glad to see Kathy have a miracle because she thought her swelling was so severe, she might not make it. She’s so exited and wants to later share her experiences with Kathy.
Again “A laymen’s description of a brain abscesses”:
“Brain abscesses commonly occur when bacteria or fungi infect part of the brain. Inflammation develops in response. Infected brain cells, white blood cells, and live and dead microorganisms collect in a limited area of the brain. This area becomes enclosed by a membrane that forms around it and creates a mass.”
Sunday, August 20, 2006
Eureka-Kathy is Back!

Unbelievable is the best way to describe today. Kathy not only came out swinging but she appears to have regained most of her mental abilities today. I don’t know how to measure her progress but she could be back to 90%-99%. She not only got her right side movements going as strong as her left side movements but seemed in control of her body too. Mentally she had it all; understanding, processing, alertness, full control of her physical functions, talking (in whispers) and even attitude. All of us were totally blown away with her responses. Physically she went all day with her pressure tube closed, ventilator removed, morphine turned off and appeared ready to come home. I have to pinch myself to remember how depressed we were yesterday and within hours she was 180 degrees different. I don’t want to get too excited about her progress but this was an outstanding day. Keep up the prayers and love, its definitely working!
Contest Question?
What does Kathleen D. Newhouse and Randy D. Haskell have in common?
Please post your answers to this comment link below-The winner will get a prize. I will give you the answers and winner's name Tuesday
Please post your answers to this comment link below-The winner will get a prize. I will give you the answers and winner's name Tuesday
Sunday-Nocturnal Sightings

I knew as soon as I would post my frustration over Kathy’s progress she would do something. The great news is that she took her agility test at 6:00 AM today and she not only did her left side good but raises her right hand to her face! She was able to raise two fingers up on both hands and wiggle both toes. Not only was the nurses excited but Kathy looked excited too. She was awake more last night than in the past few evenings. Conscious time was spent scanning her eyes around the room and starring at her fingernails. I think this was in response to Trevor telling her Saturday he would paint her fingernails bright green while she sleeping. Maybe things are looking up……I will see for myself later this morning.
Saturday, August 19, 2006
Brain Injury: Severity Levels and the Recovery Process
Prognosis
People often want to know when their loved one will get better and how much the person will recover. These are very difficult questions to answer because of many uncertainties about brain injuries. Your health care team will do their best to provide you with the most accurate estimation of recovery that they can. Sometimes, however, the most honest response will be a frustrating one: “We’ll just have to wait and see.”
Many factors affect the rate and extent of recovery after brain injury. Your loved one’s physicians will be collecting and integrating all the information available as they make their assessments. Some of these factors include pre-existing features:
the medical history of the person, age, history of previous neurological problems,
the injury itself (the type and location of the injury, the depth and duration of coma, the presence of low blood pressure or oxygen levels after the injury) and
current findings (results of physical examinations, radiological studies of the brain, etc.)
The Recovery Process
The fact that the brain recovers at all is remarkable in many ways. A brain injury causes the death of brain cells (neurons). Unfortunately, the brain is one of the few places in the body that cells do not seem to regenerate. Yet, people with brain injuries often make tremendous gains.
Scientists are still unsure about all of the mechanisms that allow for brain recovery. Possibilities include: some of the neurons are just bruised or swollen and not permanently damaged. As the bruising and swelling improve, the neurons start to function again;
other parts of the brain take over the functions of the damaged areas and new connections between the remaining brain cells may form.
Regardless of the reasons, people can get better after a brain injury. However, for the reasons mentioned, predicting the degree and pace of recovery is very difficult.
A person’s recovery after a brain injury goes through a series of stages. After severe brain injury, the sequence is:coma, coma emergence, post-traumatic amnesia and
resolution of post-traumatic amnesia.
More information about these terms follows, but keep these points in mind as you read it.
These stages represent only general categories. Sometimes, recovery can stop at one of these stages and not progress to the next stage. The transition between stages is rarely abrupt; it is usually very gradual. Every person recovers at an individual pace, so it is difficult to compare the experience of one person to another.
Much of the recovery after a brain injury occurs early after the injury – usually within the first six months. Most experts agree that the brain can continue to heal for up to two years after an injury. Even after two years, people can continue to slowly improve. The reason for this continued progress is that many of the gains after the first year or two do not depend so much on the healing of the brain, as on the learning of new skills. Although difficulties, such as muscle weakness or poor memory, may not change at this point, people who are recovering are learning ways to compensate and become more functional. The recovery process at this point is more like being back in school than recuperating from a surgery.
After a severe brain injury, the person is in a coma. This means that they are unaware and unresponsive. It is a state of unconsciousness. The person can not be described as asleep or awake; there are no sleep-wake cycles. They do not speak, follow commands or open their eyes. There are, however, stages of coma, such as lighter or deeper, and these are usually measured by the Glasgow Coma Scale (GCS), see Table 1. The higher the score is, the lighter the coma stage. A person with a score between three (which is the lowest possible score) and eight is considered in a coma.
As a person’s score improves, he or she is considered to be emerging from coma. These changes usually take place gradually. For instance, people may start to open their eyes or show evidence that they have sleep cycles, but they may still be unable to speak or follow commands. As these abilities appear, the GCS no longer applies. Most rehabilitation centers now use the Rancho Levels of Cognitive Functioning to describe the progress of the person at this point (refer to Table 2.).
The term minimally conscious state refers to people who demonstrate some (but very little) awareness and responsiveness to their surroundings. Their responses are typically inconsistent. Thus, they are not considered comatose or vegetative. As the name suggests, a person is considered conscious in this state. Occasionally, physicians may prescribe medicines that help stimulate the brain, especially if a person is not becoming more responsive with time. Some people do not progress beyond this stage in their recovery process.
Most people move beyond this stage and enter what is often referred to as post-traumatic amnesia. As the name suggests, this is a stage in which the person has serious memory problems. However, it does not refer to all problems with memory after a brain injury. Post-traumatic amnesia is a technical term that refers to the stage that people are in after emerging from coma. Its main feature is the inability to remember any information from day to day. As a result, the person with a brain injury is disoriented and confused (they do not know where they are or what has happened to them). This does not mean that a person is unable to benefit from therapies, however. Evidence exists that people are able to retain basic skills that they are taught without remembering that they learned them! This is sometimes referred to as procedural or implicit memory.
In addition to having memory problems, people in post-traumatic amnesia are often agitated. Some of this agitation is a result of the brain injury itself, and some is simply a response to the confusion a person feels at this stage. It can be a frightening experience to see a loved one during this time. It is important to remember that the behavior you see is not under the control of the person. The physicians may sometimes order medicines to help relieve some of the agitation. In addition, they may order some sort of physical restraint to prevent persons in this stage from hurting themselves or others, such as a special bed or mitts. Just as important are the other steps that the whole team will take.
Post-traumatic amnesia is thought to resolve when these people are able to consistently remember basic information from day to day. Most likely, however, they will never recover any memories from a short time before their accident through the resolution of their post-traumatic amnesia. It is also important to realize that these persons can still have significant problems with their memory even though the post-traumatic amnesia has resolved. After the resolution of post-traumatic amnesia, further recovery continues. Again, it is extremely difficult to predict just how quickly and how much recovery to expect.
If you are interested in the TABLES ( Glasgow Coma Scale and Rancho Levels Of Cognitive Functioning) please go to the following link:
http://lifecenter.ric.org/content/2162/index.html?topic=1&subtopic=271
People often want to know when their loved one will get better and how much the person will recover. These are very difficult questions to answer because of many uncertainties about brain injuries. Your health care team will do their best to provide you with the most accurate estimation of recovery that they can. Sometimes, however, the most honest response will be a frustrating one: “We’ll just have to wait and see.”
Many factors affect the rate and extent of recovery after brain injury. Your loved one’s physicians will be collecting and integrating all the information available as they make their assessments. Some of these factors include pre-existing features:
the medical history of the person, age, history of previous neurological problems,
the injury itself (the type and location of the injury, the depth and duration of coma, the presence of low blood pressure or oxygen levels after the injury) and
current findings (results of physical examinations, radiological studies of the brain, etc.)
The Recovery Process
The fact that the brain recovers at all is remarkable in many ways. A brain injury causes the death of brain cells (neurons). Unfortunately, the brain is one of the few places in the body that cells do not seem to regenerate. Yet, people with brain injuries often make tremendous gains.
Scientists are still unsure about all of the mechanisms that allow for brain recovery. Possibilities include: some of the neurons are just bruised or swollen and not permanently damaged. As the bruising and swelling improve, the neurons start to function again;
other parts of the brain take over the functions of the damaged areas and new connections between the remaining brain cells may form.
Regardless of the reasons, people can get better after a brain injury. However, for the reasons mentioned, predicting the degree and pace of recovery is very difficult.
A person’s recovery after a brain injury goes through a series of stages. After severe brain injury, the sequence is:coma, coma emergence, post-traumatic amnesia and
resolution of post-traumatic amnesia.
More information about these terms follows, but keep these points in mind as you read it.
These stages represent only general categories. Sometimes, recovery can stop at one of these stages and not progress to the next stage. The transition between stages is rarely abrupt; it is usually very gradual. Every person recovers at an individual pace, so it is difficult to compare the experience of one person to another.
Much of the recovery after a brain injury occurs early after the injury – usually within the first six months. Most experts agree that the brain can continue to heal for up to two years after an injury. Even after two years, people can continue to slowly improve. The reason for this continued progress is that many of the gains after the first year or two do not depend so much on the healing of the brain, as on the learning of new skills. Although difficulties, such as muscle weakness or poor memory, may not change at this point, people who are recovering are learning ways to compensate and become more functional. The recovery process at this point is more like being back in school than recuperating from a surgery.
After a severe brain injury, the person is in a coma. This means that they are unaware and unresponsive. It is a state of unconsciousness. The person can not be described as asleep or awake; there are no sleep-wake cycles. They do not speak, follow commands or open their eyes. There are, however, stages of coma, such as lighter or deeper, and these are usually measured by the Glasgow Coma Scale (GCS), see Table 1. The higher the score is, the lighter the coma stage. A person with a score between three (which is the lowest possible score) and eight is considered in a coma.
As a person’s score improves, he or she is considered to be emerging from coma. These changes usually take place gradually. For instance, people may start to open their eyes or show evidence that they have sleep cycles, but they may still be unable to speak or follow commands. As these abilities appear, the GCS no longer applies. Most rehabilitation centers now use the Rancho Levels of Cognitive Functioning to describe the progress of the person at this point (refer to Table 2.).
The term minimally conscious state refers to people who demonstrate some (but very little) awareness and responsiveness to their surroundings. Their responses are typically inconsistent. Thus, they are not considered comatose or vegetative. As the name suggests, a person is considered conscious in this state. Occasionally, physicians may prescribe medicines that help stimulate the brain, especially if a person is not becoming more responsive with time. Some people do not progress beyond this stage in their recovery process.
Most people move beyond this stage and enter what is often referred to as post-traumatic amnesia. As the name suggests, this is a stage in which the person has serious memory problems. However, it does not refer to all problems with memory after a brain injury. Post-traumatic amnesia is a technical term that refers to the stage that people are in after emerging from coma. Its main feature is the inability to remember any information from day to day. As a result, the person with a brain injury is disoriented and confused (they do not know where they are or what has happened to them). This does not mean that a person is unable to benefit from therapies, however. Evidence exists that people are able to retain basic skills that they are taught without remembering that they learned them! This is sometimes referred to as procedural or implicit memory.
In addition to having memory problems, people in post-traumatic amnesia are often agitated. Some of this agitation is a result of the brain injury itself, and some is simply a response to the confusion a person feels at this stage. It can be a frightening experience to see a loved one during this time. It is important to remember that the behavior you see is not under the control of the person. The physicians may sometimes order medicines to help relieve some of the agitation. In addition, they may order some sort of physical restraint to prevent persons in this stage from hurting themselves or others, such as a special bed or mitts. Just as important are the other steps that the whole team will take.
Post-traumatic amnesia is thought to resolve when these people are able to consistently remember basic information from day to day. Most likely, however, they will never recover any memories from a short time before their accident through the resolution of their post-traumatic amnesia. It is also important to realize that these persons can still have significant problems with their memory even though the post-traumatic amnesia has resolved. After the resolution of post-traumatic amnesia, further recovery continues. Again, it is extremely difficult to predict just how quickly and how much recovery to expect.
If you are interested in the TABLES ( Glasgow Coma Scale and Rancho Levels Of Cognitive Functioning) please go to the following link:
http://lifecenter.ric.org/content/2162/index.html?topic=1&subtopic=271
Saturday-Resting and Steady
Overnight Kathy slept well and the nurses were encouraged. No news is good news as her nurse’s say, so they will go about the normal course of business, feeding and turning. I’ve been frustrated over the last three days because Kathy has not progressed much mentally. The nurse reminds me not to get impatient because her brain is still very inflamed and even with low bacteria counts, the inflammation causes major problems. In addition her internal sodium retention is down (needs to be boosted) and her overall trauma can’t be overlooked. She tends to act in three specific ways, intense heavy sleeping, or short bursts of lucidity with good awareness and longer term consciousness with quick eye roaming and lack of concentration. Mentally I hoping she will improve tomorrow and into next week.
She is still receiving four IV’s of varying amounts of morphine, insulin, antibiotic and general fluid agent. She has four tubes running into her nose and mouth, a ventilator, feeding tube, gastric suction and mouth saliva suction. Nourishment is two bottles a day of Promate with fiber to satisfy hunger. (It looks so bad I want some) Still she looks like a poster child for the ICU.
It’s another slow weekend in the ICU and approaching 12 days of hospitalization not including Mexico. Dr. Kureshi seems satisfied with her progress and I hope to talk to him one on one Monday morning and get his thoughts on what is planned. I keep telling myself to be patient and don’t forget what she has gone through and what’s ahead.
She is still receiving four IV’s of varying amounts of morphine, insulin, antibiotic and general fluid agent. She has four tubes running into her nose and mouth, a ventilator, feeding tube, gastric suction and mouth saliva suction. Nourishment is two bottles a day of Promate with fiber to satisfy hunger. (It looks so bad I want some) Still she looks like a poster child for the ICU.
It’s another slow weekend in the ICU and approaching 12 days of hospitalization not including Mexico. Dr. Kureshi seems satisfied with her progress and I hope to talk to him one on one Monday morning and get his thoughts on what is planned. I keep telling myself to be patient and don’t forget what she has gone through and what’s ahead.
Friday, August 18, 2006
Physical Side Progressing
Yesterday afternoon they moved Kathy into a more private room in the ICU unit. Now that she is awake, she is more affected by the noise and commotion in ICU. The private room is much appreciated. (It has a TV!) Her physical progress continues well with yesterday morning and today’s (taken at 4:00 AM) CT scan showing good progress. Her mental improvement has hit a temporary plateau with her left side showing good signs of recovery and her right side stalling. We are all very interested in when they take out her ventilator tubes if she will be able to speak. Dr. Kureshi felt from the very start that the two areas of potential damage would be her right side movement and her speech. I will get a full update from her doctors today and the nurses hope she can get some rest today from her last two days of sleep deprivation.
Kathy spent this afternoon sleeping. She got her hair washed and a bath and fell asleep. The doctors raised her tube receptacle up to 15 cm over her head. Her pressure remained in the 8-10 range. When they get it to 20 cm and her pressure holds they will consider removing the tube. She cannot leave ICU unless the tube is out, period. Other IV’s and tubes have been removed and she is on a steady stream of liquid food. Her progress was hard to gauge because the staff was trying to let her rest today and not put her through a lot of gymnastics. She should be more rested tomorrow.
Kathy spent this afternoon sleeping. She got her hair washed and a bath and fell asleep. The doctors raised her tube receptacle up to 15 cm over her head. Her pressure remained in the 8-10 range. When they get it to 20 cm and her pressure holds they will consider removing the tube. She cannot leave ICU unless the tube is out, period. Other IV’s and tubes have been removed and she is on a steady stream of liquid food. Her progress was hard to gauge because the staff was trying to let her rest today and not put her through a lot of gymnastics. She should be more rested tomorrow.
Thursday, August 17, 2006
Kathy's Surgeon-Dr.Sohaib Kureshi
Dr. Sohaib Kureshi is the Head of the Neurology at Scripps Mercy Hospital. I went to his web page and downloaded his picture and information. Some of the information below might be dated?
Welcome to the Neurosurgical Medical Clinic. Our surgeons and nurses provide neurosurgical care in many of the major hospitals in San Diego, California. Our surgeons and staff provide individual and conscientious treatment using the most effective and modern techniques available in the world.
Dr. Sohaib Kureshi recently joined the NMC after finishing his residency at Duke University in Durham, North Carolina. He has special interests in skull base surgery and complex spinal diseases.
Secretary: Tori Rochaemail: torir@sd-neurosurgeon.com
Tel: 619 297-4481Fax: 619 295-6948Offices: Hillcrest and Chula Vista
Areas of special interest: Skull base surgery , brain tumors and stereotactic biopsy, complex spinal disorders.
Thursday's Update
Called Kathy’s night nurse this morning and she reported everything went well over the evening. She slept all night except the occasional checks by the nurse. The good news is the nurse checks showed Kathy’s right side was improving! She is off to get a CT scan today and her ulcer checked.
Visited with Kathy around noon today and she was very tired from her CT scan this morning. We are looking forward to Dr. Kureshi’s comments. They are attempting to take Kathy off her ventilator (maybe Kathy can talk afterwards) today but she is having problems remembering to breathe when she dozes off. The nurses assure me this is normal and when she clears up from the medicines she will start breathing on her own.
This afternoon the staff raised the collection container higher than Kathy’s head to slow down the flow from her brain in anticipation of orders to remove the drainage line from her head. This was good news even with increased brain pressure. The fluid is clear now and I think they are slowly removing systems from Kathy so she can moved out of ICU.
Visited with Kathy around noon today and she was very tired from her CT scan this morning. We are looking forward to Dr. Kureshi’s comments. They are attempting to take Kathy off her ventilator (maybe Kathy can talk afterwards) today but she is having problems remembering to breathe when she dozes off. The nurses assure me this is normal and when she clears up from the medicines she will start breathing on her own.
This afternoon the staff raised the collection container higher than Kathy’s head to slow down the flow from her brain in anticipation of orders to remove the drainage line from her head. This was good news even with increased brain pressure. The fluid is clear now and I think they are slowly removing systems from Kathy so she can moved out of ICU.
A Special Thank You
Without your love and support Kathy and our family would have never got through this. I appreciate the prayers and concerns by each one of you. The personal visits and support have been truly overwhelming. Thank you!
Mickey and Brian
Debbie, Bob, Jamie, Jaren and Scott
Kiki, Randy, Heath and Megan
Athene and Jonathan
Trevor and Jennifer
Mike and Erin
Ryan, Michelle and Macy
Al, Enoris, and Brian
Barbara and Jim
La Donna
Kellen and Alyssa
Dave and Jackie
Curt
Jaudiel, Maribel, Jonathan, Alondra, Jackaline
Pat, Milt, Babs, Adam and Amy
Carol and Kisa
Vicky, John, Matt and Scott
Max and Artruo
Kevin and Peter
Juan and his wife
The West Pak Family
Mickey and Brian
Debbie, Bob, Jamie, Jaren and Scott
Kiki, Randy, Heath and Megan
Athene and Jonathan
Trevor and Jennifer
Mike and Erin
Ryan, Michelle and Macy
Al, Enoris, and Brian
Barbara and Jim
La Donna
Kellen and Alyssa
Dave and Jackie
Curt
Jaudiel, Maribel, Jonathan, Alondra, Jackaline
Pat, Milt, Babs, Adam and Amy
Carol and Kisa
Vicky, John, Matt and Scott
Max and Artruo
Kevin and Peter
Juan and his wife
The West Pak Family
Wednesday, August 16, 2006
Catching Up
The purpose of this Web Blog is to keep family and friends informed of Kathy’s progress in a single easy to access web page. Whenever you want to quickly update yourself about Kathy, come to this site. You can post comments (we encourage you to do so) and it will include links and other information. Since I started this blog site early this week, I need to catch up and get current. Let’s review the highlights and lowlights from Thursday August 10th through Wednesday August 16th.
Thursday Aug 10th:
We spent the morning trying to figure out what happened. Dr. Kureshi was extremely helpful walking us through each step and what to expect over the next few days. He basically reiterated that Kathy was in severe danger from the abscess. The abnormality he originally identified in her brain CT turned out to be a burst abscess. It had burst deep inside her brain and flowed directly into her ventricles, the liquid area between the brain and the skull, circling the brain. He needed to identify the bacteria in a culture to identify for proper treatment. Over the course of the next 24 hours the team ultimately discovered the bacteria’s type and began administering penicillin. It was sad to witness all of the tubes running into Kathy. She remained unresponsive from the impact of the heavy post surgery medication. Dr. Kureshi warned us to take things day by day. He was looking to concentrate only on keeping Kathy’s brain alive.
Friday Aug 11th:
Family arrived early and spoke to Dr. Kureshi concerning Kathy’s morning condition. He was alarmed about Kathy’s sudden spike in brain pressure. (A normal brain pressure is measured in the 1-10 range and it would take standing on your head to even reach 15.) Kathy’s brain pressure was hovering around 50 and at one point had shot up to 80. He told us that without quick relief, there were only two options. Remove a section of her skull to relieve the pressure but risk heavy post surgery brain damage. The other option was even worse, the brain would eventually succumb to the pressure and Kathy’s brain would be dead. The penicillin was working but also increasing pressure by creating a high volume of puss. The drain installed into Kathy’s head was not large enough to keep up with the debris volume resulting in rising pressure. Dr. Kureshi decided to put Kathy into a medical coma to stop all of her brain activity and give her a better chance to fight the battle. We all got together afterwards, family and friends, assuming all was grave. We prayed for her survival that day.
Saturday Aug 12th:
By Saturday morning, Kathy’s pressure had dropped into the mid 20’s. Everyone was greatly relieved and our thoughts of morbidity had turned into a small ray of hope. I looked around Kathy’s bed and could not believe anyone could have more tubs and IV’s running in and out, including Phenobarbital to induce coma, Vecurionium to freeze muscle activity (paralyze) and Propful for pain and sedation. Dr. Kureshi was glad to see her pressures drop but gave us no encouraging words. It was another long night.
Sunday Aug 13th:
Sunday was a special day because many local churches had Kathy on their prayer lists and many family and friends were in attendance. Upstairs in the Hospital, Adam and Amy were having their first baby, a beautiful girl named McKenzie, to everyone’s delight and joy. The morning started great as Kathy bounced back and forth from 8 to15 pressure. Her exit tube had cleared from a white puss filled line into a lighter yellow color fluid. (The proper color is like Fiji Water-clear) We had progressed, the nurses were encouraged and everyone had a sigh of relief. The on-call nurses felt Kathy’s elevated heart rate was telling them she was in pain and began administering Morphine too. On Saturday both nurses hinted that more activity from the doctors could occur Monday morning. Maybe something that would give a hint about her mental state? Things looked good when late Sunday they administered that last bag of Phenobarbital. Get up early tomorrow-we got news to hear.
Monday Aug 14th
We all got to the hospital early hoping for a sighting of her Neurologists. This was the day we were going to know something! That idea flew out the windows immediately when Dr. Kureshi told us he decided to slowly step down the removal of Kathy’s medications as not to upset her delicate balance. Suddenly we realized she would take days not hours to get out of her coma. The good news was her pressure had dropped into single digits and her fluid color was light yellow. The nurses that afternoon removed the Phenobarbital station completely and started to crank down the Vecurionium and the Propful. Hurry up and wait.
Tuesday Aug 15th
I called early Tuesday morning and the night nurse said everything was doing about as good as possible. Pressure continued to stay low and her brain fluid was getting lighter and lighter. Dr. Kureshi was in morning surgery as we waited to soak up any news. He finally showed and again reminded us that Kathy would take days and days to awake from her narcotic induced sleep. The afternoon wore on and I visited Kathy just before the shift change. I was denied entrance at first because of all the commotion of a just arriving gunshot victim. I finally got in but all the emergency nurses were attending the shooting victim. I went straight to talk to Kathy and out of the blue she opened both her eyes, scarring me. I could tell immediately she recognized me and my voice. I was so shocked and happy I could not contain myself! The nurses returned and confirmed that Kathy had awakened and passed some recognition tests. I rushed out and called everyone immediately and it was great to hear the excitement on everyone’s voice. Our Kathy was back and not one second to soon.
Wednesday Aug 16th:
The morning was a whirlwind of activity as everyone came by to see Kathy’s awake. The nurse warned us not to get her too excited and not to ask her to move parts of her body for us because that was her job not ours. Kathy had improved lucidity this morning and her range of motion had improved from last night. She not only showed us selected fingers, but had strong hand movement and some movement in her legs. The left side of her body is much better than the right. She favors her left and the nurse prescribed that we do all we can to get her to greet us on the right side. Anyway, that would be addressed in her physical therapy sessions. Dr. Kureshi stopped by in the afternoon and was very positive. He said he was “greatly encouraged” by Kathy’s recovery. Combine that with our nurse commenting “she had never seen anything like her recovery in 25 years” made us feel like nothing else.
Tonight Kathy was sleeping from her long day of visitors. I came in around 8:00 PM and she awoke to me and made good eye contact. She reached up and grabbed my hand acknowledging I was there. Her night doctors came by and were concerned about a little stomach bleeding (ulcer) that appeared this afternoon. Besides the possible ulcer they spent most of the time reviewing other medical issues, not her brain, so it appears there focus is more on her general health than just her head. What a great drive home! We love you Kathy.
Thursday Aug 10th:
We spent the morning trying to figure out what happened. Dr. Kureshi was extremely helpful walking us through each step and what to expect over the next few days. He basically reiterated that Kathy was in severe danger from the abscess. The abnormality he originally identified in her brain CT turned out to be a burst abscess. It had burst deep inside her brain and flowed directly into her ventricles, the liquid area between the brain and the skull, circling the brain. He needed to identify the bacteria in a culture to identify for proper treatment. Over the course of the next 24 hours the team ultimately discovered the bacteria’s type and began administering penicillin. It was sad to witness all of the tubes running into Kathy. She remained unresponsive from the impact of the heavy post surgery medication. Dr. Kureshi warned us to take things day by day. He was looking to concentrate only on keeping Kathy’s brain alive.
Friday Aug 11th:
Family arrived early and spoke to Dr. Kureshi concerning Kathy’s morning condition. He was alarmed about Kathy’s sudden spike in brain pressure. (A normal brain pressure is measured in the 1-10 range and it would take standing on your head to even reach 15.) Kathy’s brain pressure was hovering around 50 and at one point had shot up to 80. He told us that without quick relief, there were only two options. Remove a section of her skull to relieve the pressure but risk heavy post surgery brain damage. The other option was even worse, the brain would eventually succumb to the pressure and Kathy’s brain would be dead. The penicillin was working but also increasing pressure by creating a high volume of puss. The drain installed into Kathy’s head was not large enough to keep up with the debris volume resulting in rising pressure. Dr. Kureshi decided to put Kathy into a medical coma to stop all of her brain activity and give her a better chance to fight the battle. We all got together afterwards, family and friends, assuming all was grave. We prayed for her survival that day.
Saturday Aug 12th:
By Saturday morning, Kathy’s pressure had dropped into the mid 20’s. Everyone was greatly relieved and our thoughts of morbidity had turned into a small ray of hope. I looked around Kathy’s bed and could not believe anyone could have more tubs and IV’s running in and out, including Phenobarbital to induce coma, Vecurionium to freeze muscle activity (paralyze) and Propful for pain and sedation. Dr. Kureshi was glad to see her pressures drop but gave us no encouraging words. It was another long night.
Sunday Aug 13th:
Sunday was a special day because many local churches had Kathy on their prayer lists and many family and friends were in attendance. Upstairs in the Hospital, Adam and Amy were having their first baby, a beautiful girl named McKenzie, to everyone’s delight and joy. The morning started great as Kathy bounced back and forth from 8 to15 pressure. Her exit tube had cleared from a white puss filled line into a lighter yellow color fluid. (The proper color is like Fiji Water-clear) We had progressed, the nurses were encouraged and everyone had a sigh of relief. The on-call nurses felt Kathy’s elevated heart rate was telling them she was in pain and began administering Morphine too. On Saturday both nurses hinted that more activity from the doctors could occur Monday morning. Maybe something that would give a hint about her mental state? Things looked good when late Sunday they administered that last bag of Phenobarbital. Get up early tomorrow-we got news to hear.
Monday Aug 14th
We all got to the hospital early hoping for a sighting of her Neurologists. This was the day we were going to know something! That idea flew out the windows immediately when Dr. Kureshi told us he decided to slowly step down the removal of Kathy’s medications as not to upset her delicate balance. Suddenly we realized she would take days not hours to get out of her coma. The good news was her pressure had dropped into single digits and her fluid color was light yellow. The nurses that afternoon removed the Phenobarbital station completely and started to crank down the Vecurionium and the Propful. Hurry up and wait.
Tuesday Aug 15th
I called early Tuesday morning and the night nurse said everything was doing about as good as possible. Pressure continued to stay low and her brain fluid was getting lighter and lighter. Dr. Kureshi was in morning surgery as we waited to soak up any news. He finally showed and again reminded us that Kathy would take days and days to awake from her narcotic induced sleep. The afternoon wore on and I visited Kathy just before the shift change. I was denied entrance at first because of all the commotion of a just arriving gunshot victim. I finally got in but all the emergency nurses were attending the shooting victim. I went straight to talk to Kathy and out of the blue she opened both her eyes, scarring me. I could tell immediately she recognized me and my voice. I was so shocked and happy I could not contain myself! The nurses returned and confirmed that Kathy had awakened and passed some recognition tests. I rushed out and called everyone immediately and it was great to hear the excitement on everyone’s voice. Our Kathy was back and not one second to soon.
Wednesday Aug 16th:
The morning was a whirlwind of activity as everyone came by to see Kathy’s awake. The nurse warned us not to get her too excited and not to ask her to move parts of her body for us because that was her job not ours. Kathy had improved lucidity this morning and her range of motion had improved from last night. She not only showed us selected fingers, but had strong hand movement and some movement in her legs. The left side of her body is much better than the right. She favors her left and the nurse prescribed that we do all we can to get her to greet us on the right side. Anyway, that would be addressed in her physical therapy sessions. Dr. Kureshi stopped by in the afternoon and was very positive. He said he was “greatly encouraged” by Kathy’s recovery. Combine that with our nurse commenting “she had never seen anything like her recovery in 25 years” made us feel like nothing else.
Tonight Kathy was sleeping from her long day of visitors. I came in around 8:00 PM and she awoke to me and made good eye contact. She reached up and grabbed my hand acknowledging I was there. Her night doctors came by and were concerned about a little stomach bleeding (ulcer) that appeared this afternoon. Besides the possible ulcer they spent most of the time reviewing other medical issues, not her brain, so it appears there focus is more on her general health than just her head. What a great drive home! We love you Kathy.
Picture of Intraventricular Rupture (File Photo)

MRI shows the abscess communicating
and discharging, through a tract, into the
ipselateral ventricle. Intraventricular rupture of
an abscess is usually a catastrophic event leading
to ventriculitis and dissemination of organisms
throughout the cerebrospinal fluid pathway.
This event accounts for the calamitous
deterioration in the patient’s clinical condition.
Text Book Medical Analysis
Definition
Brain abscess is a bacterial infection within the brain.
Description
The brain is usually well insulated from infection by bacteria, protected by the skull, the meninges (tissue layers surrounding the brain), the immune system, and the highly regulated barrier between the bloodstream and the brain. Under certain circumstances, however, bacteria can invade the brain and cause a localized infection called an abscess. Brain abscess is relatively rare, accounting for 1 in 10,000 hospital admissions. Single abscess occurs in 75% of cases, and the remainder of cases involve multiple abscesses. If not treated, brain abscess is almost always fatal.
Causes and symptoms
One-half of all brain abscesses are caused by the spread of bacteria from a nearby infection. Sources of bacteria include:
middle ear infections (otitis media) or infections in the bony spaces in front of the middle ear (mastoiditis)
sinus infections
an abscessed tooth.
other sources of bacteria include:
lung infections
abdominal infection
infection of the heart's lining (endocarditis)
penetrating head wounds
Brain abscess can be caused by a variety of organisms, many of them related to ear and sinus infections. Many times brain abscess cases are caused by two or more bacteria. In 30-60% of cases, the bacteria combination includes streptococci, microorganisms that can live without oxygen (anaerobes), and enterobacteria. A small number of cases are caused by yeast, fungi, and single-cell organisms (protozoa).
The symptoms of brain abscess often develop slowly, usually within a period of about two weeks. The most common symptoms are:
headache
neurologic symptoms related to the specific part of the brain that is infected
altered mental status
seizures
Fever and stiff neck occur in less than one-third of cases. Additional symptoms may include vomiting, eye tremor (nystagmus), poor balance, and uncoordinated movements.
Diagnosis
Diagnosis of brain abscess is performed by using a computed tomography scan (CT) or a magnetic resonance imaging (MRI) scan to determine the site of infection. Tissue removal (biopsy) is usually performed as well. A biopsy is performed to determine the type of bacterium involved. Biopsies can also be used to rule out tumor or other noninfectious localized lesions, which may look the same on the scans.
Other tests are performed to determine the source of the infection. These tests include blood cultures, x rays of the chest, and a physical exam of the ears, sinuses, and teeth. A test for human immunodeficiency virus (HIV) is usually also performed.
Treatment
Treatment for brain abscess begins with intravenous antibiotics, chosen to match the infecting bacterium if known, or to cover a wide spectrum of possibilities if not. Treatment usually continues for six to eight weeks.
Aspiration surgery is almost always done to drain the abscess. In this procedure, a needle is guided to the infected site by CT scan, and fluid is removed (aspirated) from the abscess. Aspiration may be repeated several times until the bacteria are completely killed or removed. Surgical removal of infected or dead tissue may be needed in some cases. For patients with many sites of infection, aspiration or surgical removal is not done because of the increased difficulty and risk of the procedure. For these patients, antibiotic therapy alone is used. Steroid treatment is controversial, but may be indicated in some cases.
Prognosis
Even with prompt treatment, brain abscess is fatal in about 20% of cases. About half of those who survive have some residual neurological problems, including seizures in many patients.
There are several reasons why patients with brain abscess can have a poor prognosis. The illness may not be diagnosed correctly or an accurate diagnosis may take additional time. The patient may receive an antibiotic that does not match the infecting organism. Sometimes the infection may not be limited to a definite area in the brain, making diagnosis and treatment difficult. The small number of cases caused by fungal infection may take additional time to diagnose. A patient may also have a poor prognosis because there is more than one abscess, the location of the abscess may be deep within the brain, or the infection may have moved into many locations within the brain. Severe complications can result from brain abscess, including comma and brain rupture. In 80-100% of cases involving brain rupture, the patient dies.
Prevention
Brain abscess may be preventable by prompt and aggressive treatment of the infections which give rise to it, especially sinus and ear infections.
Key Terms
Biopsy
The removal of a tissue sample for examination.
Aspiration
Removal of fluid from a closed space through a needle.
For Your Information
Books
Harrison's Principles of Internal Medicine. Ed. Anthony S. Fauci, et al. New York: McGraw-Hill, 1997.
Rolak, Loren A. "Brain and Spinal Abscesses." In Office Practice of Neurology, ed. Martin Samuels and Steven Feske. New York: Churchill Livingstone, 1996.
Wispelwey, Brian, and Carole A. Sable. "Intracranial Suppuration." In Current Therapy of Infectious Disease, ed. David Schlossberg. St. Louis: Mosby-Year Book, 1996.
Brain abscess is a bacterial infection within the brain.
Description
The brain is usually well insulated from infection by bacteria, protected by the skull, the meninges (tissue layers surrounding the brain), the immune system, and the highly regulated barrier between the bloodstream and the brain. Under certain circumstances, however, bacteria can invade the brain and cause a localized infection called an abscess. Brain abscess is relatively rare, accounting for 1 in 10,000 hospital admissions. Single abscess occurs in 75% of cases, and the remainder of cases involve multiple abscesses. If not treated, brain abscess is almost always fatal.
Causes and symptoms
One-half of all brain abscesses are caused by the spread of bacteria from a nearby infection. Sources of bacteria include:
middle ear infections (otitis media) or infections in the bony spaces in front of the middle ear (mastoiditis)
sinus infections
an abscessed tooth.
other sources of bacteria include:
lung infections
abdominal infection
infection of the heart's lining (endocarditis)
penetrating head wounds
Brain abscess can be caused by a variety of organisms, many of them related to ear and sinus infections. Many times brain abscess cases are caused by two or more bacteria. In 30-60% of cases, the bacteria combination includes streptococci, microorganisms that can live without oxygen (anaerobes), and enterobacteria. A small number of cases are caused by yeast, fungi, and single-cell organisms (protozoa).
The symptoms of brain abscess often develop slowly, usually within a period of about two weeks. The most common symptoms are:
headache
neurologic symptoms related to the specific part of the brain that is infected
altered mental status
seizures
Fever and stiff neck occur in less than one-third of cases. Additional symptoms may include vomiting, eye tremor (nystagmus), poor balance, and uncoordinated movements.
Diagnosis
Diagnosis of brain abscess is performed by using a computed tomography scan (CT) or a magnetic resonance imaging (MRI) scan to determine the site of infection. Tissue removal (biopsy) is usually performed as well. A biopsy is performed to determine the type of bacterium involved. Biopsies can also be used to rule out tumor or other noninfectious localized lesions, which may look the same on the scans.
Other tests are performed to determine the source of the infection. These tests include blood cultures, x rays of the chest, and a physical exam of the ears, sinuses, and teeth. A test for human immunodeficiency virus (HIV) is usually also performed.
Treatment
Treatment for brain abscess begins with intravenous antibiotics, chosen to match the infecting bacterium if known, or to cover a wide spectrum of possibilities if not. Treatment usually continues for six to eight weeks.
Aspiration surgery is almost always done to drain the abscess. In this procedure, a needle is guided to the infected site by CT scan, and fluid is removed (aspirated) from the abscess. Aspiration may be repeated several times until the bacteria are completely killed or removed. Surgical removal of infected or dead tissue may be needed in some cases. For patients with many sites of infection, aspiration or surgical removal is not done because of the increased difficulty and risk of the procedure. For these patients, antibiotic therapy alone is used. Steroid treatment is controversial, but may be indicated in some cases.
Prognosis
Even with prompt treatment, brain abscess is fatal in about 20% of cases. About half of those who survive have some residual neurological problems, including seizures in many patients.
There are several reasons why patients with brain abscess can have a poor prognosis. The illness may not be diagnosed correctly or an accurate diagnosis may take additional time. The patient may receive an antibiotic that does not match the infecting organism. Sometimes the infection may not be limited to a definite area in the brain, making diagnosis and treatment difficult. The small number of cases caused by fungal infection may take additional time to diagnose. A patient may also have a poor prognosis because there is more than one abscess, the location of the abscess may be deep within the brain, or the infection may have moved into many locations within the brain. Severe complications can result from brain abscess, including comma and brain rupture. In 80-100% of cases involving brain rupture, the patient dies.
Prevention
Brain abscess may be preventable by prompt and aggressive treatment of the infections which give rise to it, especially sinus and ear infections.
Key Terms
Biopsy
The removal of a tissue sample for examination.
Aspiration
Removal of fluid from a closed space through a needle.
For Your Information
Books
Harrison's Principles of Internal Medicine. Ed. Anthony S. Fauci, et al. New York: McGraw-Hill, 1997.
Rolak, Loren A. "Brain and Spinal Abscesses." In Office Practice of Neurology, ed. Martin Samuels and Steven Feske. New York: Churchill Livingstone, 1996.
Wispelwey, Brian, and Carole A. Sable. "Intracranial Suppuration." In Current Therapy of Infectious Disease, ed. David Schlossberg. St. Louis: Mosby-Year Book, 1996.
Tuesday, August 15, 2006
Surgery and Post Surgery
The emergency staff performed a CAT Scan and a MRI of the Kathy's head upon arrival. It became clear that activity in Kathy's brain was adnormal and she would need to have surgery. Trevor signed the releases and she was rushed into surgery that afternoon.
Her capable surgeon, Dr. Sohaib Kureshi, head of Neurological Surgery at Scripps Mercy Hospital was her operating doctor. (Everything was performed on Wednesday the 9th)After surgery Dr. Kureshi explained to Trevor that Kathy had a abscess in a difficult to reach area far inside her brain. It was in fact so deep, he would never attempt to extricate it. That was not the end of the bad news, it got only worse. The abscess had burst the day earlier and spread bacteria around her brain and the brain ventricles. This action resulted in the term "ventricilitus", which is the extremely dangerous infection of the fluid surrounding the brain cavity. Because this infection in the brain also creates pressure, he needed to drill a hole in Kathy's skull to relieve the pressure and keep the brain from being permantley damaged.
Of course we were all devastated upon hearing the news. Being new to the complexities of her condition we did not fully appreciate the high morality rate of this infection. All we could do was pray and hoped for a speedy recovery.
Her capable surgeon, Dr. Sohaib Kureshi, head of Neurological Surgery at Scripps Mercy Hospital was her operating doctor. (Everything was performed on Wednesday the 9th)After surgery Dr. Kureshi explained to Trevor that Kathy had a abscess in a difficult to reach area far inside her brain. It was in fact so deep, he would never attempt to extricate it. That was not the end of the bad news, it got only worse. The abscess had burst the day earlier and spread bacteria around her brain and the brain ventricles. This action resulted in the term "ventricilitus", which is the extremely dangerous infection of the fluid surrounding the brain cavity. Because this infection in the brain also creates pressure, he needed to drill a hole in Kathy's skull to relieve the pressure and keep the brain from being permantley damaged.
Of course we were all devastated upon hearing the news. Being new to the complexities of her condition we did not fully appreciate the high morality rate of this infection. All we could do was pray and hoped for a speedy recovery.
What happened?
Most of you know the events surrounding Kathy's sudden brain abscess and sickness. This post is for the people who want more details. Kathy started to get a strong headache on Wednesday, August the 2nd. She has had a long history of migraines and she thought it was just another. Her pain got worse each day and her prescription for migraines, Imitrix was not working.
It was Saturday and I asked Kellen, my son to take her to the emergency room in Fallbrook. I was busy at work trying to finish up loose ends before our family vacation/work trip to Mexico began that Monday. We were all concerned her headache and was it going to be too strong to make the trip? Kellen took her to emergency room and she spent 6 hours in the Fallbrook hospital. The doctors focused on her migraine and treated her with a IV and a prescription for vicodine to break the cycle. We could not get her prescription for some reason that night and she had a rough night. I went to the pharmacy early the next day and she took the vicodine and felt better on Sunday.
We departed for Mexico on Monday as planned and Kathy seemed much improved and only complained of a light headache. We traveled all day and arrived into Ixtapa around 6:00 PM that evening. She was tired but feeling better. We all went to dinner that night and did not retire until around 11:00 PM. The next morning (Tuesday the 8th) I was awakened to her loud complaints of a bad headache and extreme stomach pain. I though maybe she had gotten food poisoning from dinner or the stomach flu. I called the hotel doctor and she came over immediately to look at Kathy. I told her about her migraines and the pain she was suffering. The doctor, Dr. Olivia Montifar seemed capable and very caring. She gave her pain medication and ordered prescriptions for her headache (Imitix) and for her stomach issues. Kathy seemed to calm down for a while and I was hoping the worse was over. Around 1:00PM she started acting unusual, delirious and non-responsive. I was befuddled. Finally my daughter came up to the room and helped me control her so I could contact the doctor. We both decided to take her to the hospital immediately. Kathy fought us for over a hour trying to get her to the car.
Finally we got her into the car and took her to the nearby Naval Hospital (actual Mexican Navy Hospital) and meet her original doctor, Dr. Montifar. They admitted her to large, clean private room and the nurses prepared Kathy for her stay. The doctors first administered medications for her high temperature and performed lab tests to check for e-coli virus or flu virus. About four hours later the results came in and Kathy checked out negative and her temperature had dropped to normal.
Unfortunately, other bad things were going on inside her head. Her eyes became dilated, rolling back into her head and she could no longer respond to her name or identify me or the kids. It was 8:00 PM and the doctor suggested I should consider immediately taking her to a better equipped hospital in Mexico City or transport her back to the United States. The doctors were mainly worried about her worsening mental condition over the last 4 hours. I decided at that moment to get Kathy back to the United States ASAP and I called our emergency medical evacuation number. Medex Assist kicked in and arranged a medical-evacuation for the next morning. She remained delirious all night and I was really scarred about her survival.
The emergency evacuation team arrived at the hospital at 7:30 AM sharp(Wednesday the 9th). She was taken by ambulance to the Ixtapa airport and a special Lear jet was standing by with two EMT doctors to accompany her on the flight. My daughter got on board and they both headed back to Brown Field in San Diego. Another ambulance was waiting there to take Kathy to Scripps Mercy Hospital-Trauma Unit and they arrived at 12:30 PM. She was taken into emergency ICU immediately. My son Trevor meet the ambulance at Scripps and gave the ICU doctors the history of the events and her current meds. What a relief she was back in the USA-thank god!
It was Saturday and I asked Kellen, my son to take her to the emergency room in Fallbrook. I was busy at work trying to finish up loose ends before our family vacation/work trip to Mexico began that Monday. We were all concerned her headache and was it going to be too strong to make the trip? Kellen took her to emergency room and she spent 6 hours in the Fallbrook hospital. The doctors focused on her migraine and treated her with a IV and a prescription for vicodine to break the cycle. We could not get her prescription for some reason that night and she had a rough night. I went to the pharmacy early the next day and she took the vicodine and felt better on Sunday.
We departed for Mexico on Monday as planned and Kathy seemed much improved and only complained of a light headache. We traveled all day and arrived into Ixtapa around 6:00 PM that evening. She was tired but feeling better. We all went to dinner that night and did not retire until around 11:00 PM. The next morning (Tuesday the 8th) I was awakened to her loud complaints of a bad headache and extreme stomach pain. I though maybe she had gotten food poisoning from dinner or the stomach flu. I called the hotel doctor and she came over immediately to look at Kathy. I told her about her migraines and the pain she was suffering. The doctor, Dr. Olivia Montifar seemed capable and very caring. She gave her pain medication and ordered prescriptions for her headache (Imitix) and for her stomach issues. Kathy seemed to calm down for a while and I was hoping the worse was over. Around 1:00PM she started acting unusual, delirious and non-responsive. I was befuddled. Finally my daughter came up to the room and helped me control her so I could contact the doctor. We both decided to take her to the hospital immediately. Kathy fought us for over a hour trying to get her to the car.
Finally we got her into the car and took her to the nearby Naval Hospital (actual Mexican Navy Hospital) and meet her original doctor, Dr. Montifar. They admitted her to large, clean private room and the nurses prepared Kathy for her stay. The doctors first administered medications for her high temperature and performed lab tests to check for e-coli virus or flu virus. About four hours later the results came in and Kathy checked out negative and her temperature had dropped to normal.
Unfortunately, other bad things were going on inside her head. Her eyes became dilated, rolling back into her head and she could no longer respond to her name or identify me or the kids. It was 8:00 PM and the doctor suggested I should consider immediately taking her to a better equipped hospital in Mexico City or transport her back to the United States. The doctors were mainly worried about her worsening mental condition over the last 4 hours. I decided at that moment to get Kathy back to the United States ASAP and I called our emergency medical evacuation number. Medex Assist kicked in and arranged a medical-evacuation for the next morning. She remained delirious all night and I was really scarred about her survival.
The emergency evacuation team arrived at the hospital at 7:30 AM sharp(Wednesday the 9th). She was taken by ambulance to the Ixtapa airport and a special Lear jet was standing by with two EMT doctors to accompany her on the flight. My daughter got on board and they both headed back to Brown Field in San Diego. Another ambulance was waiting there to take Kathy to Scripps Mercy Hospital-Trauma Unit and they arrived at 12:30 PM. She was taken into emergency ICU immediately. My son Trevor meet the ambulance at Scripps and gave the ICU doctors the history of the events and her current meds. What a relief she was back in the USA-thank god!
Subscribe to:
Posts (Atom)
